Acid Reflux and Heartburn
Everyone occasionally has heartburn. This occurs when stomach acid flows backward into the esophagus, the food pipe that carries food to the stomach. People usually experience heartburn after meals as a burning sensation or pain behind the breast bone. Often, regurgitation of food and bitter-tasting stomach acid accompanies heartburn. Antacids or milk temporarily relieves heartburn for most people.
- Why Does Heartburn Occur?
-
To understand heartburn, let us look at the body's anatomy. The esophagus carries food and liquid to the stomach. A sphincter, or muscular valve, is located at the end of the esophagus at the border between the esophagus and stomach. Known as the lower esophageal sphincter (LES) this muscle contracts much the same as the anus does. The sphincter should maintain a certain pressure to keep the end of the esophagus closed so that stomach juices are not admitted. The LES muscle should only open when food is passed into the stomach.
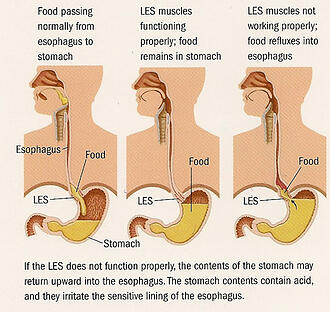
However, the LES muscle does not always work perfectly. It is felt that the problem is with inappropriate, transient relaxations of this sphincter valve that result in reflux. Sphincter function can be easily overcome by a number of factors, the most common being eating a large meal. Along with swallowed air, a large meal causes an upward pressure in the stomach to rise, thereby overpowering the LES muscle. Other factors that reduce the LES pressure and allow reflux are:
- Nicotine (cigarettes)
- Fried or fatty foods
- Chocolate
- CoffeeCitrus fruits and juices
- Peppermint
- Pregnancy
- Lying flat
- Hiatus hernia
- Certain prescription medications


- Heartburn is common, but is it serious?
-
Heartburn and reflux are extremely common, with 10 percent of the population experiencing them daily. Twenty-five percent of pregnant women have heartburn. Even though heartburn is common, it is rarely life threatening. Severe cases, however, can result in injury to the lower esophagus that requires treatment.
- What is a Hiatus Hernia?
-
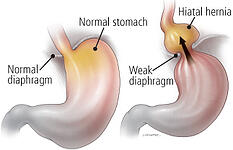
The esophagus passes through a muscle, called the diaphragm, which separates the lungs from the abdomen. When the opening in the diaphragm enlarges, a portion of the stomach can protrude (herniate) through it into the chest. This is called a hiatal hernia. A persistent hiatal hernia may produce significant heartburn. Many people with a hiatus hernia do not experience heartburn. However, 40-50% of patients with a hiatal hernia have reflux. A hiatal hernia and GERD can occur independently from one another.
- Complications and Unusual Presentations
-
Besides heartburn, the other major problems that can develop with reflux are:
- Chronic bleeding and anemia.
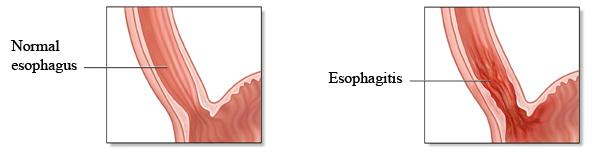
- Scar formation and narrowing, known as a stricture, of the lower esophagus which may cause swallowing difficulty or a complete blockage preventing the passage of food. A stricture usually can be treated by a stretching procedure of the area referred to as dilatation.
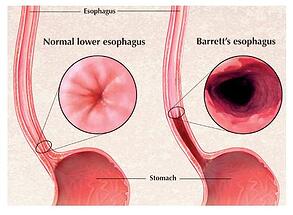
- Barrett's Esophagus, which occurs when long-term reflux irritates the lower esophagus so that the stomach lining actually grows into the esophagus. In these cases, there is a small, but definite, risk of a subsequent malignancy. Barrett's Esophagus requires periodic monitoring with endoscopy to detect early cancer states. The BARRX ablation procedure is a safe and effective treatment for Barrett's Esophagus resulting in an elimination of the abnormal tissue. You can read more here.
- Eosinophilic Esophagitis (EE) EE was first reported over 3 decades ago and has had an increasing incidence. It has a seasonal incidence that is greatest in the late summer and fall. It is an allergic,inflammatory response in the esophagus with an infiltration of eosinophils (inflammatory cells) in the lining of the esophagus. EE can present with reflux-like symptoms of heartburn, pain, or swallowing difficulty. Adults with EE often present with swallowing difficulty to solids and have a history of recurrent food impaction (food getting stuck). EE patients are treated for reflux and may require topical steroid treatment. These patients should undergo allergic testing followed by appropriate dietary manipulations and eliminations. Unfortunately, recurrence of symptoms in EE is the rule rather than the exception.
- Lung problems when reflux of stomach fluid trickle into the breathing tubes, causing wheezing, bronchitis and even pneumonia. Reflux is considered the third most common cause of asthma and cough.
- Gastroesphageal Reflux (GERD) and Laryngopharyngeal Reflux (LPR)During gastroesophageal reflux, the acidic stomach contents may travel backwards all the way up the esophagus, beyond the upper esophageal sphincter (the ring of muscle at the top of the esophagus), and into the back of the throat and possibly into the back of the nasal airway. This condition is known as laryngopharyngeal reflux (LPR), which can affect anyone. Adults with LPR often complain that the back of their throat has a bitter taste. They can also have a sensation of burning or something being “stuck.” Some may have difficulty breathing if the voice box is affected. LPR patients can suffer from chronic hoarseness, voice fatigue, and loss of vocal range. LPR can be difficult to treat and usually requires long-term medical therapy.
- Diagnosis
-
The primary tests used to diagnose reflux are:
- Upper GI Endoscopy- The patient is mildly sedated and a flexible videoscope is inserted into the esophagus to visually inspect it and the stomach
- Upper GI Series- The patient drinks liquid barium and x-rays are taken of the esophagus and stomach showing how they function.
- Esophageal manometry- This test measures the pressure within the esophagus, especially the LES pressure.
- Monitoring for Acid Reflux Detection
-
- 24 hour Ambulatory combined pH (acid)and impedance Monitoring- Ambulatory combined pH and impedance monitoring, called the Sleuth System is the new gold standard for objectively assessing nonacid as well acid reflux activity and can confirm significant gastroesophageal reflux disease. Studies show that patients with persistent symptoms on medical therapy have nonacid reflux 40% of the time. pH and impedance reflux monitoring is usually performed prior to any antireflux procedure and is used to diagnose difficult or atypical reflux cases. A tiny tube is placed through the nose and into the esophagus (food tube) above the lower esophageal sphincter. The test runs for 24 hours and measures the number of times acid enters the esophagus. Wireless technology called The BRAVO System is also available. Click here to learn more about BRAVO. BRAVO is a wireless transmitting capsule which is placed usually following endoscopy. It will measure acid reflux activity only for 48 hours and the capsule will usually fall off within 3 to 5 days and is passed. Bravo offers longer data collection times and better patient comfort, but is limited in that it only measures acid reflux activity and will not measure nonacid reflux. The newer Sleuth and Zephyr pH-impedance reflux testing that measures nonacid and acid reflux is available through Greenwich Village Gastroenterology.
- Treatment
-
General measures the patient can take to reduce reflux are:
- Eat smaller and more frequent meals.
- Avoid eating before going to bed.
- Eliminate excessive bending, lifting, abdominal exercises, girdles and tight belts, all of which increase abdominal pressure and provoke reflux.
- If overweight, lose weight. Being overweight promotes reflux.
- Eliminate the use of nicotine (cigarettes), fatty foods, alcohol, all coffees (yes-including decaf), chocolate and peppermint.
- Elevate the head of the bed 8" to 10" by placing pillows or a wedge under the upper part of the mattress. In this way, gravity keeps stomach juices out of the esophagus while the patient sleeps. It is not enough to use two pillows under the head.
- Prescription medications - check with the physician regarding side effects of prescription drugs. Some drugs actually lower the strength of the LES muscle.
- Other Treatments include:
-
- Antacids- These can and should be used more often. Generally, antacids should be taken 30 to 60 minutes after eating and at bedtime. Liquids are preferred to tablets, with the strongest being Maalox II, Mylanta II, Gelusil II and Extra Strength Riopan.
- Alginic Acid and Antacids- Two products, Gaviscon and Algicon, place a layer of foam over the fluid in the stomach to prevent reflux. These tablets should be chewed well and used 30 to 60 minutes after eating and at bedtime.
- Drugs- Medicines are now available that effectively reduces and even eliminates the secretion of stomach acid and increases the strength of the LES muscle. These medicines represent the most important method of treating reflux next to surgical or futuristic nonsurgical methods of correcting reflux.
- Laparoscopic Surgery- Surgery can treat reflux. Those patients who are dependent on acid lowering agents may entertain an antireflux procedure. There are few patients who do not respond to medical therapy and benefit from antireflux procedures. Generally, however, a failure of medical therapy is not an indication for surgery. Prior to any corrective procedure, a patient must undergo an extensive evaluation. The objective of this surgery is to strengthen the LES muscle. Successful surgery greatly relieves and can correct severe reflux and heartburn. A method of performing anti-reflux surgery is by laparoscopic technique whereby the surgery is accomplished through tiny holes in the belly button and upper abdomen. Recovery is quicker with this technique. However, the procedure is still an invasive surgery which has certain inherent risks and potential complications, and requires the use of general anesthesia. This operation should only be performed by qualified surgeons thoroughly familiar with it.
- Endoscopic, Incisionless treatments
-
Transoral Incisionless Fundoplication (TIF)
- Incisionless, nonsurgical, endoscopic assisted methods for the treatment of reflux are now available. This procedure, referred to as EsophyX (or TIF) involves the use of devices that intensify and remodel the antireflux barrier at the level of the lower sphincter valve between the esophagus and stomach. The approach to this type of surgery is through the mouth and without any cutting or incisions in the abdominal wall. The EsophyX employs a suturing and fastening system to create pleats in order the improve the lower valve function.
The team at Lenox Hill Hospital was the first center in the New York City metropolitan area to offer the EsophyX TIF (Transoral Incisionless Fundoplication). The EsophyX TIF procedure is also available at other hospital affiliations that include The Langone New York University Medical Center and Beth Israel Medical Center. Working in conjunction with the developers and manufacturers of the endoscopic reflux therapy devices, we have taken the lead in the diagnosis and management of gastroesophageal reflux disease.
Learn more about EsophyX!
Stretta
Stretta® Therapy is an other minimally invasive treatment for gastroesophageal reflux disease (GERD), the condition that causes chronic heartburn and regurgitation. If you are taking prescription anti-reflux medications such as proton pump inhibitors [PPIs] (Prilosec, Prevacid, Nexium, etc...) or H2-receptor antagonist drugs (Tagamet, Zantac, Pepcid), and you are not achieving good control of your symptoms, you may benefit from additional therapies that may be available to you, such as Stretta Therapy.
Stretta is a minimally invasive, outpatient procedure that takes approximately 60 minutes to perform. Patients usually receive conscious sedation (the same sedation used for your endoscopy procedure) and an instrument is passed through the mouth, so there are no visible cuts or scars that result from the procedure. Through a special tube, a special type of energy is delivered to the deep muscle layer of the lower esophageal sphincter that is responsible for preventing reflux. Through a remodeling process, the muscle becomes less floppy (compliant) thereby improving function.
Learn more about Stretta
- In Summary…
-
Heartburn occurs so commonly that it is normal for everyone to experience it sometime. However, when heartburn is persistent, it needs to be evaluated, and long-term follow up care is often required. Heartburn occurring two times weekly or more warrants a medical evaluation.
Medical treatment along with lifestyle changes are usually very effective and can prevent complications. For those patients requiring long-term, chronic medical therapy, an antireflux procedure, such as EsophyX or Stretta, offer a viable and usually successful alternative to more invasive surgeries or a life-long need to take drug therapies that are not always successful.
To learn more about your treatment options you may contact our offices at:
212-673-2721 or 845-471-1354 or 1-877-4GERDMD .

55 Montgomery St. Poughkeepsie, NY 12601
212 673 2721 845 471 1354
info@starpoli.com
